Medicaid Enrollment Automation Streamlines The Member Journey

In 2020, millions of people lost their insurance coverage and became eligible to enroll in Medicaid. In New York, Medicaid enrollment increased by 18.1% between March and December 2020, leaving insurers scrambling to onboard new members and comply with many other regulations. Thanks to an ongoing enrollment modernization program, Healthfirst was ready.
Prior to the pandemic, Healthfirst, New York’s largest not-for-profit health insurer, had embarked on an enrollment modernization project using the Pega platform and its intelligent automation capabilities. Those improvements and implementations helped the insurer serve its customer base in areas hard hit by the pandemic.
Healthfirst operates in a unique business model, sponsored by downstate New York’s leading hospital systems, and serves a larger community of participating hospitals and healthcare providers. The collaborative insurer-provider relationship model enables them to provide access to high-quality care for members while efficiently managing medical costs and other expenses to maximize state
reimbursements.

“Our mission is to connect New Yorkers to high quality health care, and our emerging vision is that we have to make healthcare easier, which means that we can get members seamlessly enrolled and continuously enrolled in coverage,”Healthfirst selected the Pega platform to transform enrollment processes for all stakeholders to support this membercentric transformation. The goal was to improve agility and process efficiency to serve clients better while optimizing the data flow for Healthfirst and providers. “Most provider organizations wouldn’t meet the minimum viable experience in other industries like financial services, so we wanted to make it easier for providers because if it’s better for providers, then customers will have better experiences as well,” Sweeney said. Rulesware has supported Healthfirst throughout its transformation, bringing thought leadership and guiding the client to implement the solution leveraging the power of Pega to provide intelligent automation, guided user processes and process transparency. “Rulesware differentiated themselves with their approach to enabling us to achieve our business objectives,” Sweeney said. “They have a rich and mature offering that helped bring this business process orchestration and automation vision to life. They had a reputation as being the best in the Pega ecosystem.”
– G.T. Sweeney, Healthfirst CIO
Healthfirst by the numbers
- 1.7 million members (1 in 6 New York City residents)
- 4 million enrollment annual transactions
- 15 major health systems and hospital sponsors
- 80+ participating hospitals
- 40,000 providers
- 4,500+ employees
AGILITY IN ACTION
With 1.7 million members, and growing, any changes in their legacy systems can still take considerable time. Healthfirst wanted an agile platform that allowed it to adapt quickly to situations without impacting access for members and providers. As the response to the pandemic took shape, the Pega foundation allowed Healthfirst to pivot quickly to meet its obligations under fast-changing requirements. “Pega is the market-leading tool in terms of business process orchestration and business process automation, and that’s what we needed,” Sweeney said. “We had to invest in supporting the scale we were at the time and also continue to drive growth – we are three times the membership now compared to when I joined, but we’re far more than three times as complex as we were then.” For example: Healthfirst added more than 250,000 members within a few weeks in 2020 while holding operational costs flat. Much of the volume was nonstandard transactions that required waiving re-certification and other rule changes under COVID-related mandates. While handling large non-standard volumes, the Pega automation enabled Healthfirst to keep processing times brief so members would have timely access to care.
For example: Healthfirst added more than 250,000 members within a few weeks in 2020 while holding operational costs flat. Much of the volume was nonstandard transactions that required waiving re-certification and other rule changes under COVID-related mandates. While handling large non-standard volumes, the Pega automation enabled Healthfirst to keep processing times brief so members would have timely access to care.
“The investments that we made with Rulesware as our partner to streamline the way we enroll our members and manage their continuous enrollment allowed us to efficiently absorb that membership growth,”Healthfirst initially focused on Medicaid (MCD) enrollment. Rulesware’s guidance included devising a solution that not only met the needs of MCD but also built a foundation with reuse in mind. When other high-priority needs arose mid-project, the team was able to pivot and leverage the foundation to quickly implement solutions for Nursing Home Reimbursement and Managed Long Term Care disenrollment. Each solution was implemented within six weeks from requirements to full production.
– G.T. Sweeney, Healthfirst CIO

“Our primary orientation was to modernize our approach to business processes backed by both orchestration and automation,” Sweeney said. “The management of business rules is a critical element, especially in an environment where the pace of change continues to increase.”
The platform’s agility was further proven when Healthfirst met a New York Department of Health mandate to onboard 2,500 foster care children onto Medicaid Managed Care. Finally, Healthfirst leveraged the MCD foundation when building out the next products in the plan, Qualified Health Plans (QHP) and Essential Plans (EP).
PROCESS OPTIMIZATION PAYS OFF
With more than 4 million transactions each year, enrollment processing efficiency and accuracy are among the critical KPIs for Healthfirst managers.
The MCD 834 EDI transaction set defines the information required for the Benefit Enrollment and Maintenance documents. Accuracy in gathering and transmitting member data is essential to ensure members receive benefits in a timely fashion. The system must identify and correct any errors, such as overwriting date ranges, sequencing issues or incorrect data before the enrollment batch data is ingested.
With Pega, Healthfirst improved the MCD 834 processing to a 98% first-pass rate, up from 86%. At the same time, the processing speed for a 5,000-unit batch dropped from 20 to 40 minutes down to 7 to 8 minutes.
Pega delivered a similar gain in processing for Qualified Health Plans and Essential Plans. The first pass success rate jumped from 80% to 95% in 16 weeks.
Overall, the system has automated 98% of enrollment transactions. These operational efficiencies allow Healthfirst to keep costs low without negatively impacting customer service levels.
Enrollment Transformation
- Added 250K members at a flat cost
- 98% transactions automated
- 98% first pass rate
- Batch processing 65% faster
- QHP/EP first rate 95%
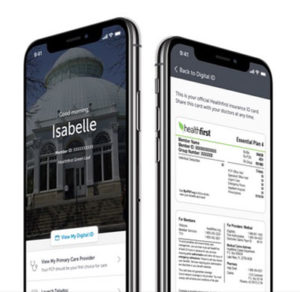
EMBRACING THE MEMBER’S JOURNEY
“In addition to helping our members navigate through the crisis, there were opportunities for us to be better on the other side of the pandemic, so we intentionally accelerated some of our strategies for making healthcare easier for consumers.”Like many other organizations, Healthfirst made the change to a member-centric approach a core part of their journey. The goal is to improve customer engagement by separating the applicant experience from the member experience. The fast, accurate processing has reduced the time it takes for members’ coverage to take effect so they can gain access to services faster. Members can choose a primary care physician on the first day of coverage, which reduces the impact of not receiving appropriate services or medications. Ensuring that initial enrollment is accurate dramatically reduces the need for costly customer services calls and escalations for resolution. Through their partnership with Pega and Rulesware, Healthfirst has succeeded in its digital transformation, enabling the organization to respond quickly to COVID-19. The shift will continue as Healthfirst strives to be more agile and responsive as it serves its members and healthcare providers. “I didn’t want just a Pega body shop; I wanted a strategic partner who could help me stand up the governance over this and at the same time knew how to bring agile to life,” Sweeney said. “Adaptability and agility are not just words in IT anymore. They’re words that we use in our corporate strategy as we transitioned from business transformation to a digital enablement orientation.”
– G.T. Sweeney, Healthfirst CIO
About Rulesware Ranked number one in Pega quality implementations, Rulesware increases profitability and operational agility for modern organizations. By unlocking streamlined compliance, appealing customer journeys, and best-in-class automation, Rulesware gives modern leaders the nextgeneration digital tools needed to master today’s most competitive markets – positioning them to succeed today and tomorrow.


