Rulesware’s Pega Expertise Takes Palomar Growth to the Next Level
Palomar, a specialty insurance provider, had plans for multiple new technology enhancements. Their in-house team was working hard to meet these goals, along with an offshore vendor. The problem? The vendor wasn’t deeply experienced with Pega, was on the other side of the globe, and was providing code that wasn’t up to Palomar’s high standards. These core challenges needed to be addressed to get to the next level.

Palomar’s use of technology is a key differentiator. Unlike older insurance companies using outdated legacy technology, Palomar relies on Pega and other proprietary systems to analyze and disseminate information quickly, which means policies get quoted and bound very quickly and accurately.
Pega is the backbone for Palomar’s policy administration system, which integrates policy issuance, underwriting, billing and portfolio analytics.
Using this unique technology platform, they provide seamless integration
into the point-of-sale systems of their distribution partners (agents, wholesale brokers, and program administrators).
An orchestrated workflow allows Palomar to rapidly quote and bind policies as well as run detailed risk-management analytics in real time. In addition to boosting speed, their technology platform provides a competitive advantage in product distribution, risk management, and reinsurance purchases.
The Challenge
THE SOLUTION
Rulesware was selected for having both deep Pega expertise and being located in a convenient nearshore time zone. Positive results were seen immediately – Palomar’s Pega compliance score increased and projects moved forward quickly. What started as a test engagement quickly grew, and today, Rulesware and Palomar work hand-in-hand on a variety of fast-moving projects. The partnership has been very rewarding for both teams.Expertise Matters
Rulesware’s 16+ years of experience with Pega has contributed to the team’s success in a big way.
Tracy says: “One of the first things we noticed with Rulesware was that they brought real expertise—this was not a team we were simply telling what to do. They came in with strong development and QA ideas and expert advice.
For example, when Rulesware first came to our office and were doing their onboarding, a couple of them were immediately deep into reading all of our old architecture materials. They studied that stuff and then came to our meetings and asked a ton of questions. They were very proactive and really cared and put the effort into understanding our product and how they could provide the most value quickly. The unexpected benefit from that kind of attitude is that we get more collaboration. We get to challenge each other to be our best.”
Benefits of Nearshore
And those late night phone calls? A thing of the past.
With Rulesware’s nearshore model— Rulesware’s specialized Pega consultants are located in the US and Latin America—time zones are no longer an issue. Agile delivery now happens at speed in real-time and everyone is in the same meetings.
“Today the Rulesware team is really just an embedded part of our team,” says Mark. “They’re participating, giving feedback and part of everything we’re doing; they’re just a seamless part of the team. And that works so much better for us than your typical ‘throw the requirement over the wall to offshore and see what comes back’ route.”
“Yes,” adds Tracy, “One of the things that I really love about our partnership is that you drop into a meeting and you can’t tell who’s internal and who’s external. Everyone treats each other with mutual respect, there’s great camaraderie; we’re in all the same meetings together. It’s just all around a really good working culture.”
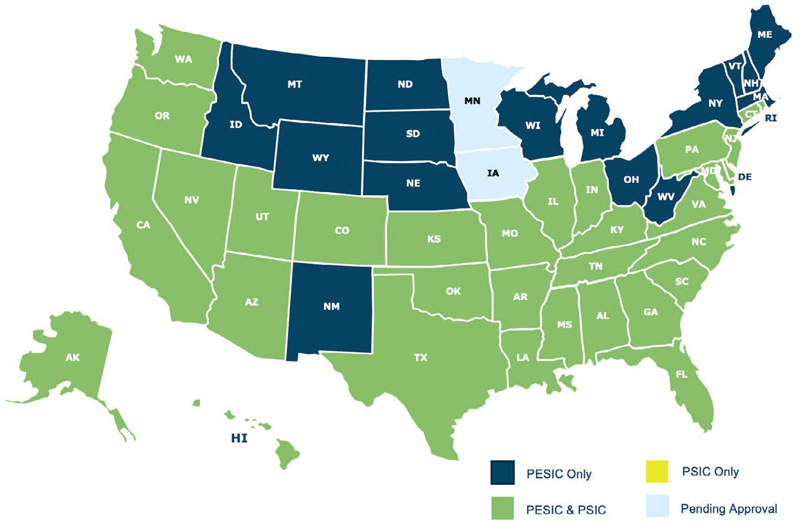
Palomar Geographic Footprint
“Rulesware hires really smart people who have delivered. There’s no bait and switch.”
-Tracy Mosel, Director of IT Program/Product Management
THE RESULT
Today Palomar and Rulesware make a highly effective team. Morale within the team is high, Palomar’s Pega compliance score has increased, products are now released quickly and accurately, and Palomar’s customers can get quotes generated and policies bound faster than ever.
“Rulesware hires really smart people who have delivered for Palomar,” says Tracy. “There’s no bait and switch; we work with an efficient team that cares about our products. We’re so happy they’re part of our team.”
Looking Ahead
Going forward, Palomar plans to continue to invest in proprietary technology assets that deepen their competitive advantage in the market. They believe that the success of their business is centered upon their relentless commitment to apply technology to improve the speed, ease and accuracy they can bring to every customer interaction and that Pega is a big part of that equation.
“We have plans to use Pega even more going forward,” says Mark. “There will be additional policy administration products, and I also see us potentially extending the reach of what we’re using Pega for with things like customer service and onboarding.”
The future looks bright for Palomar, and Rulesware is proud to be a valued partner along the way.